Periodontics
Satisfied Smiles since 1984
First in Restorative, Aesthetic & Implant Dentistry
631.669.2330
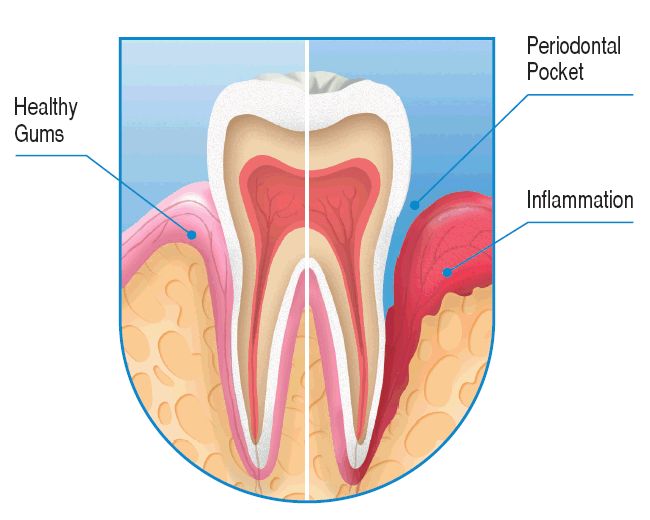
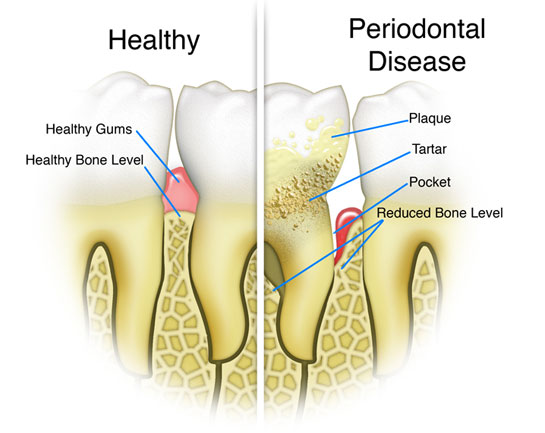
What is Periodontal Disease?
Periodontal disease is often silent, meaning symptoms may not appear until an advanced stage of the disease. However, warning signs of periodontal disease include the following:
- Red, swollen or tender gums or other pain in your mouth
- Bleeding while brushing, flossing, or eating hard food
- Gums that are receding or pulling away from the teeth, causing the teeth to look longer than before
- Loose or separating teeth
- Pus between your gums and teeth
- Sores in your mouth
- Persistent bad breath
- A change in the way your teeth fit together when you bite
- A change in the fit of partial dentures
Smoking/Tobacco Use
As you probably already know, tobacco use is linked with many serious illnesses such as cancer, lung disease and heart disease, as well as numerous other health problems. What you may not know is that tobacco users also are at increased risk for periodontal disease. In fact, recent studies have shown that tobacco use may be one of the most significant risk factors in the development and progression of periodontal disease.
Genetics
Puberty, Pregnancy and Menopause in Women
Stress
Medications
Clenching or Grinding Your Teeth
Diabetes
Other Systemic Diseases
Poor Nutrition and Obesity
Non-Surgical Treatments
Most dental professionals would agree that after scaling and root planing, many patients do not require any further active treatment, including surgical therapy. However, the majority of patients will require ongoing maintenance therapy to sustain health. Non-surgical therapy does have its limitations, however, and when it does not achieve periodontal health, surgery may be indicated to restore periodontal anatomy damaged by periodontal diseases and to facilitate oral hygiene practices.
Heart Disease
Several theories exist to explain the link between periodontal disease and heart disease. One theory is that oral bacteria can affect the heart when they enter the bloodstream, attaching to fatty plaques in the coronary arteries (heart blood vessels) and contributing to clot formation. Coronary artery disease is characterized by a thickening of the walls of the coronary arteries due to the buildup of fatty proteins. Blood clots can obstruct normal blood flow, restricting the amount of nutrients and oxygen required for the heart to function properly. This may lead to heart attacks.
Another possibility is that the inflammation caused by periodontal disease increases plaque build-up, which may contribute to swelling of the arteries. Researchers have found that people with periodontal disease are almost twice as likely to suffer from coronary artery disease as those without periodontal disease. Periodontal disease can also exacerbate existing heart conditions. Patients at risk for infective endocarditis may require antibiotics prior to dental procedures. Dr. Proto and your cardiologist will be able to determine if your heart condition requires the use of antibiotics prior to dental procedures.
